- Appointments
- Sunnybank 07 3344 1440
- Mater Health Hub 07 3041 5082
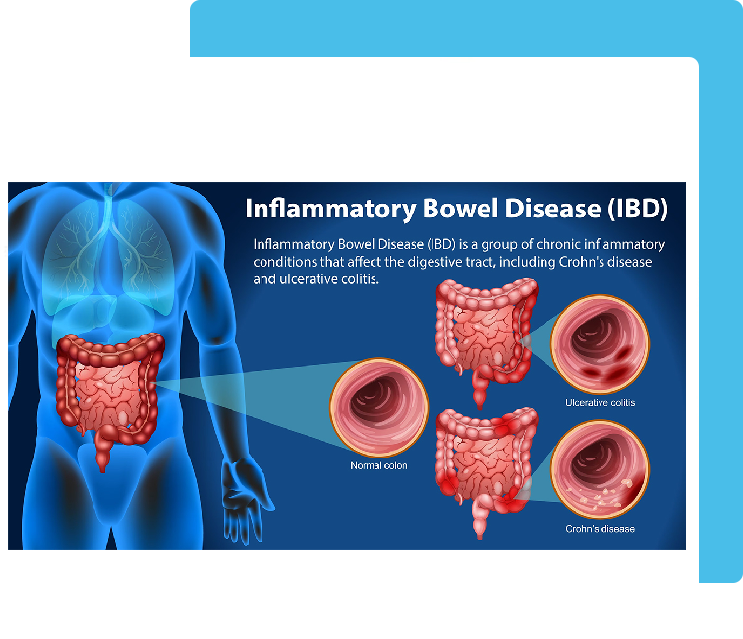
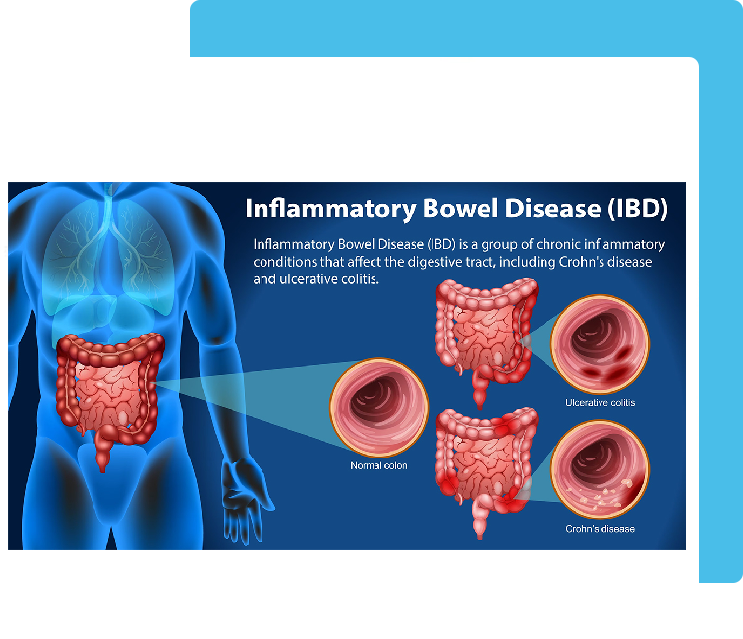
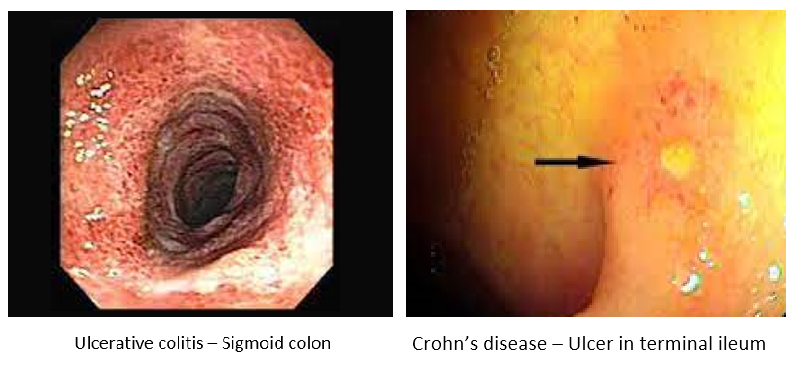
Inflammatory bowel disease (IBD) is a group of disorders that cause chronic inflammation in the intestines. IBD includes Crohn’s disease and ulcerative colitis. Both types can affect multiple systems in the body, Digestive system is the most commonly affected.
Inflammatory bowel disease symptoms vary, depending on the severity of inflammation and where it occurs. Symptoms may range from mild to severe. You are likely to have periods of active illness followed by periods of remission. For some, it can be a debilitating condition that can lead to life-threatening complications.
Both ulcerative colitis and Crohn's disease usually are characterized by diarrhea, Blood in the stools, abdominal pain, fatigue, reduced appetite and weight loss.
Rarely, IBD can cause fever, Join pain, itchy red painful eyes, vision problem, Jaundice and skin rashes. If inflammation is not controlled, over the time it can damage the intestines and can cause abscess, stricture, fistula, bowel obstruction and increases the risk of developing bowel cancer.
IBD usually appears as a sudden flare-up of symptoms. Most people diagnosed with IBD are age 35 or younger. There is a second peak of diagnosis in the 60s.
There is no single test to diagnose IBD. Because the symptoms of IBD overlap with those of several other conditions, including infections and other digestive system disorders, your doctor may recommend a combination of the following to confirm the diagnosis:
Although there is no curative treatment for IBD, it’s possible to reduce inflammation and address symptoms with a variety of therapies. The goals of treating IBD include stopping future flare-ups and healing inflammation in the intestines. Because IBD often causes issues in different parts of the body, a multispecialty approach is required.
IBD treatments may include medications ( Anti-inflammatory, Immunosuppressants, antibiotics, steroids, biological therapy etc) and a range of diet and lifestyle changes that help reduce inflammation and support the immune system. Surgery is required if medical therapy fails or there is a complication from IBD like abscess, fistula, stricture, perforation, bowel obstruction or bowel cancer.
All Copyrights © 2023 Dr. Kaushik Kumar
Powered by :: Growup Business Solution